Understanding Vasovagal Syncope: Causes, Symptoms, and Treatment
Vasovagal syncope is a common condition characterized by a sudden loss of consciousness resulting from a temporary decrease in blood flow to the brain. In this article, we will delve into the intricacies of vasovagal syncope, exploring its causes, symptoms, and available treatment options.
What is Vasovagal Syncope?
Vasovagal syncope, also known as neurocardiogenic syncope or reflex syncope, is a type of fainting episode that occurs due to a sudden drop in blood pressure and heart rate. It is the most common form of syncope, accounting for approximately 50% of all reported cases. While it can affect individuals of all ages, vasovagal syncope tends to be more prevalent in younger individuals, especially adolescents.
Defining Vasovagal Syncope
Vasovagal syncope is a result of the body’s autonomic nervous system overreacting to certain triggers. The autonomic nervous system regulates various bodily functions, including heart rate, blood pressure, and digestion. In individuals with vasovagal syncope, certain triggers can cause a sudden malfunction in the autonomic nervous system, leading to a decrease in blood flow to the brain and subsequent loss of consciousness.
Common triggers for vasovagal syncope include prolonged standing, dehydration, extreme emotional distress, pain, and even the sight of blood. These triggers can stimulate the autonomic nervous system in susceptible individuals, resulting in a cascade of events that lead to fainting. Understanding these triggers is crucial in managing and preventing vasovagal syncope episodes.
Prevalence of Vasovagal Syncope
As mentioned earlier, vasovagal syncope is highly prevalent, with various studies estimating its occurrence in around 3-4% of the general population. While it can affect individuals of all demographics, it tends to be more common in younger individuals, particularly females. The exact reasons for this gender disparity are still uncertain and require further investigation.
Studies have also shown a potential genetic component to vasovagal syncope, with a higher likelihood of experiencing syncope if a close family member also has a history of fainting episodes. This suggests a possible hereditary predisposition to the condition, although more research is needed to fully understand the genetic factors at play.
The Anatomy of Vasovagal Syncope
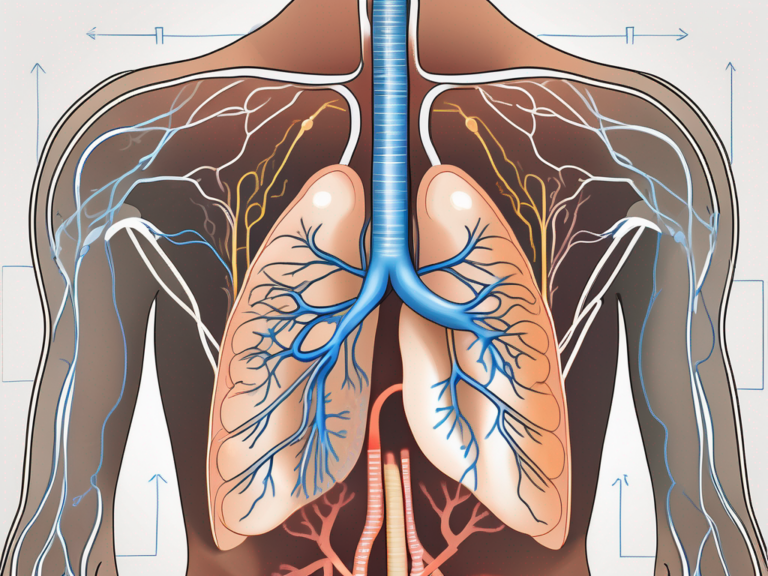
Understanding the underlying mechanisms of vasovagal syncope requires an insight into the intricate workings of the human body, particularly the involvement of the vagus nerve.
Vasovagal syncope, also known as neurocardiogenic syncope, is a common cause of fainting episodes. It occurs when there is a sudden drop in blood pressure and heart rate, leading to a temporary loss of consciousness. While the exact triggers for vasovagal syncope can vary from person to person, common factors include emotional stress, pain, dehydration, and standing for long periods.
The Role of the Vagus Nerve
The vagus nerve, also known as the tenth cranial nerve, plays a vital role in the regulation of various bodily functions, including heart rate and blood pressure. In individuals with vasovagal syncope, an exaggerated response of the vagus nerve can occur in response to specific triggers. This abnormal response leads to a sudden drop in blood pressure and heart rate, thereby causing a temporary loss of consciousness.
Furthermore, the vagus nerve is responsible for the parasympathetic nervous system, which is often referred to as the “rest and digest” system. It helps regulate involuntary bodily functions such as digestion, breathing, and heart rate. Dysfunction of the vagus nerve can lead to a range of symptoms beyond syncope, including gastrointestinal issues, heart rhythm abnormalities, and difficulty swallowing.
The Body’s Response to Vasovagal Syncope
When an individual experiences a vasovagal syncope episode, the body initiates a series of physiological responses as a result of the drop in blood flow to the brain. These responses include dilation of blood vessels, increased heart rate, and increased resistance in blood vessels. These compensatory mechanisms aim to restore blood flow to the brain and prevent further complications.
It is important to note that while vasovagal syncope is typically not a serious condition, recurrent episodes can impact an individual’s quality of life. Treatment options may include lifestyle modifications, such as increasing fluid intake and avoiding triggers, as well as medications to help regulate blood pressure and heart rate. In severe cases, medical interventions such as pacemakers or implantable loop recorders may be considered to manage symptoms and prevent fainting episodes.
Causes of Vasovagal Syncope
Vasovagal syncope can be triggered by a variety of factors, ranging from emotional stress to physical changes in the body. While the exact cause may vary from individual to individual, certain common triggers have been identified.
Vasovagal syncope, also known as neurocardiogenic syncope, occurs when the body overreacts to certain triggers, leading to a sudden drop in heart rate and blood pressure. This can result in a temporary loss of consciousness, often accompanied by symptoms such as dizziness, lightheadedness, and nausea.
Common Triggers for Vasovagal Syncope
Some of the common triggers for vasovagal syncope include:
- Emotional stress or anxiety
- Prolonged standing or sitting in one position
- Pain or the sight of blood
- Exposure to heat or crowded environments
- Sudden unexpected pain or fright
- Vigorous physical activity or exercise
It is important to note that while these triggers can provoke a vasovagal response in susceptible individuals, the exact mechanism behind why some people experience syncope in response to these stimuli is not fully understood.
Underlying Health Conditions and Vasovagal Syncope
In addition to the aforementioned triggers, certain underlying health conditions can predispose individuals to vasovagal syncope. These conditions include:
- Heart rhythm abnormalities
- Neurological disorders
- Anemia
- Dehydration
- Diabetes
- Medications that affect blood pressure
Individuals with preexisting heart conditions, such as arrhythmias or structural heart abnormalities, may be more prone to experiencing vasovagal syncope. Similarly, those with autonomic nervous system disorders, such as postural orthostatic tachycardia syndrome (POTS), may also be at an increased risk.
Recognizing the Symptoms of Vasovagal Syncope
Recognizing the symptoms of vasovagal syncope is crucial for prompt identification and appropriate management of the condition. Vasovagal syncope, also known as neurocardiogenic syncope, is a common cause of fainting episodes and is characterized by a sudden drop in heart rate and blood pressure, leading to a temporary loss of consciousness.
Understanding the diverse array of symptoms associated with vasovagal syncope can help individuals and healthcare professionals better recognize and respond to episodes of syncope.
Physical Symptoms of Vasovagal Syncope
The physical symptoms of vasovagal syncope may vary from individual to individual but commonly include:
- Lightheadedness or dizziness
- Blurry vision or tunnel vision
- Feeling warm or sweating excessively
- Nausea or vomiting
These physical symptoms are often the body’s way of signaling a drop in blood flow to the brain, which can trigger the fainting response in individuals with vasovagal syncope.
Emotional and Cognitive Symptoms
In addition to the physical symptoms, individuals experiencing a vasovagal syncope episode may exhibit emotional and cognitive symptoms such as:
- Feeling anxious or fearful
- Experiencing panic or confusion
- Temporary loss of memory or disorientation
These emotional and cognitive symptoms can be distressing for individuals experiencing syncope, adding to the overall complexity of the condition. It is important for individuals and their caregivers to be aware of these additional symptoms to provide appropriate support during and after an episode of vasovagal syncope.
Diagnosing Vasovagal Syncope
Accurate diagnosis of vasovagal syncope requires a comprehensive evaluation, including examination of medical history and specialized diagnostic tests.
When it comes to vasovagal syncope, a condition characterized by a sudden drop in heart rate and blood pressure leading to fainting, the diagnostic process can be intricate. Understanding the patient’s medical history is crucial in unraveling the underlying factors contributing to their syncopal episodes. By delving into the specifics of the symptoms experienced, potential triggers, and any preexisting health conditions, healthcare providers can piece together a more complete picture of the individual’s health.
Medical History and Vasovagal Syncope
The first step in diagnosing vasovagal syncope involves taking a detailed medical history. This includes a discussion of the patient’s symptoms, triggers, and any underlying health conditions that may contribute to the episodes. Often, a careful history can provide valuable clues and help guide further diagnostic investigations.
Moreover, understanding the patient’s lifestyle habits, such as their level of physical activity, stress levels, and hydration status, can offer additional insights into the potential triggers for vasovagal syncope. Factors like dehydration, prolonged standing, or stressful situations can all play a role in precipitating an episode, underscoring the importance of a holistic approach to diagnosis.
Diagnostic Tests for Vasovagal Syncope
In some cases, further diagnostic tests may be necessary to confirm the diagnosis of vasovagal syncope and rule out other underlying causes. These tests may include:
- Electrocardiogram (ECG)
- Tilt-table test
- Echocardiogram
- Blood tests
- Electrophysiological study (EPS)
Each of these tests serves a specific purpose in evaluating different aspects of cardiac function, electrical activity, and overall health. For example, an ECG can detect irregular heart rhythms, while a tilt-table test can assess how the body responds to changes in position. By combining the information gathered from the medical history with the results of these diagnostic tests, healthcare providers can formulate a more targeted treatment plan tailored to the individual needs of the patient.
Treatment Options for Vasovagal Syncope
While there is no definitive cure for vasovagal syncope, several treatment options are available to manage the condition and reduce the frequency and severity of syncope episodes.
Vasovagal syncope, also known as neurocardiogenic syncope, is a common cause of fainting episodes. It occurs when the body overreacts to certain triggers, leading to a sudden drop in heart rate and blood pressure, resulting in a temporary loss of consciousness. Managing vasovagal syncope involves a combination of lifestyle changes, medications, and in some cases, surgical interventions.
Lifestyle Changes to Manage Vasovagal Syncope
Implementing certain lifestyle modifications can be effective in managing vasovagal syncope. These include:
- Staying hydrated
- Avoiding triggers such as prolonged standing
- Gradually changing positions to prevent sudden drops in blood pressure
- Wearing compression stockings to improve blood circulation
- Maintaining a balanced diet
Furthermore, incorporating regular exercise into your routine can help improve cardiovascular health and reduce the frequency of syncope episodes. Engaging in activities such as yoga or Pilates can also be beneficial, as they focus on breathing techniques and gentle movements that promote relaxation and stress reduction.
Medications for Vasovagal Syncope
In some cases, healthcare professionals may prescribe medications to help manage vasovagal syncope. These medications may include:
- Beta-blockers to regulate heart rate and blood pressure
- Fludrocortisone to increase blood volume
- Selective Serotonin Reuptake Inhibitors (SSRIs) to manage anxiety and panic symptoms
- Antidepressants to help regulate blood pressure
It is important to work closely with your healthcare provider to determine the most suitable medication and dosage for your specific condition. Regular monitoring and adjustments may be necessary to ensure optimal management of vasovagal syncope.
Surgical Treatments for Vasovagal Syncope
In rare cases where other treatment options prove ineffective, surgical interventions may be considered. These may include the implantation of a pacemaker to regulate heart rhythm or the surgical removal of the overactive vagus nerve.
Surgical treatments are typically reserved for individuals with severe and debilitating symptoms that significantly impact their quality of life. It is essential to discuss the potential risks and benefits of surgical interventions with your healthcare team to make an informed decision about the most appropriate course of action.
Living with Vasovagal Syncope
Vasovagal syncope can significantly impact an individual’s quality of life and daily activities. However, with appropriate management techniques and a proactive approach, individuals can learn to cope with the condition and lead fulfilling lives.
Coping Mechanisms for Vasovagal Syncope
Developing effective coping mechanisms can help individuals navigate and manage the challenges posed by vasovagal syncope. Some strategies that may prove useful include:
- Learning relaxation techniques such as deep breathing and meditation
- Maintaining a support network and seeking emotional support from loved ones
- Engaging in regular physical exercise to promote overall cardiovascular health
- Tracking triggers and avoiding situations that precipitate syncope
Living with vasovagal syncope requires a multifaceted approach that goes beyond the management of symptoms. It is important for individuals to understand the underlying mechanisms of the condition and how it affects their body. By gaining knowledge about vasovagal syncope, individuals can feel more empowered and in control of their own health.
In addition to the coping mechanisms mentioned above, it is also beneficial for individuals to make certain lifestyle modifications. This may include maintaining a well-balanced diet, staying hydrated, and avoiding excessive alcohol or caffeine consumption. These lifestyle changes can help regulate blood pressure and reduce the likelihood of syncope episodes.
Prognosis and Quality of Life with Vasovagal Syncope
While vasovagal syncope can be disruptive and distressing, it is essential to recognize that most individuals with the condition have a good prognosis. With appropriate management strategies and a proactive approach, individuals can achieve an improved quality of life and minimize the impact of syncope episodes.
It is important to note that the prognosis may vary from person to person, depending on the severity of their symptoms and their response to treatment. Some individuals may experience infrequent and mild episodes, while others may have more frequent and severe episodes. However, with the right combination of lifestyle modifications, medications, and medical interventions, the majority of individuals can effectively manage their condition and lead fulfilling lives.
In conclusion, understanding vasovagal syncope involves recognizing the causes, symptoms, and available treatment options. While it can be challenging to navigate, the condition can be effectively managed through a combination of lifestyle modifications, medications, and surgical interventions in select cases. By adopting appropriate coping mechanisms, making lifestyle modifications, and seeking support, individuals can lead a fulfilling and empowered life despite the challenges posed by vasovagal syncope.