The Importance of the Mandibular Nerve
The mandibular nerve, a branch of the trigeminal nerve, plays a vital role in the functioning of the jaw and the surrounding areas. Understanding the importance of this nerve is crucial for dental professionals, scientists, and anyone interested in oral health and pain management.
Understanding the Mandibular Nerve
Located within the lower jaw, the mandibular nerve is responsible for providing sensation to the lower teeth, chin, lower lip, and gums. It also supplies motor fibers to the muscles involved in chewing. By understanding the anatomy of the mandibular nerve, we can gain valuable insights into its functions and potential disorders.
The mandibular nerve, also known as the inferior alveolar nerve, is a crucial component of the trigeminal nerve, one of the major nerves responsible for sensation in the face. It plays a vital role in facilitating various functions essential for daily activities such as eating, speaking, and facial expressions. Understanding the intricate network of the mandibular nerve can shed light on the complexities of facial sensation and motor control.
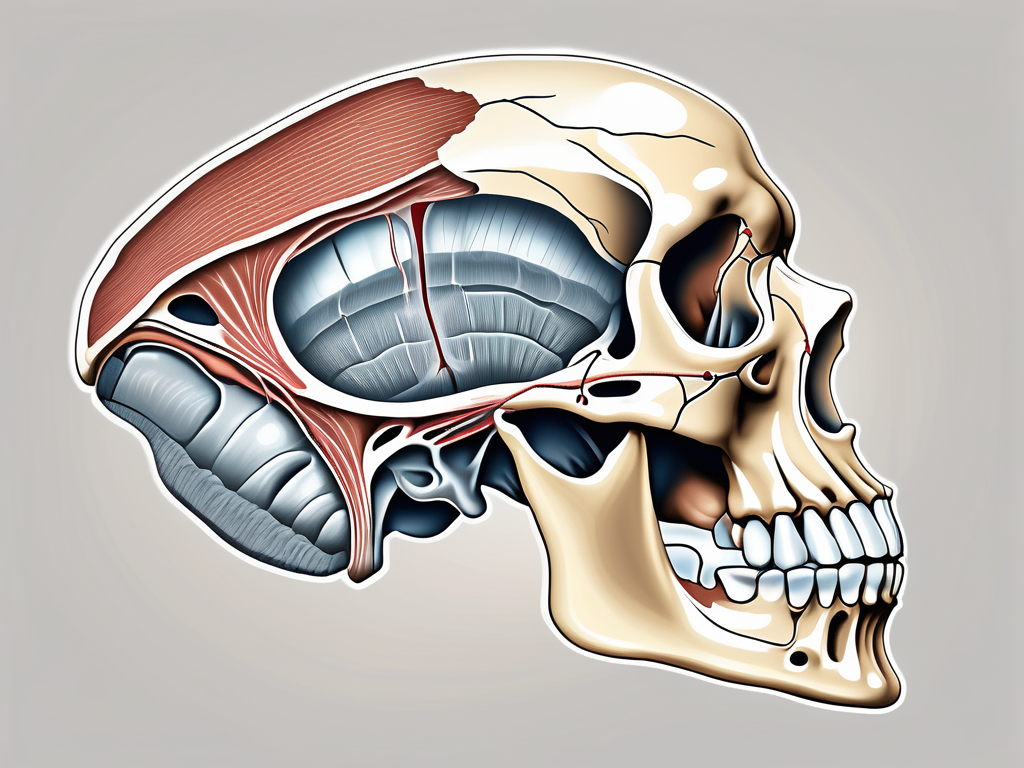
Anatomy of the Mandibular Nerve
The mandibular nerve begins within the skull, specifically in the trigeminal ganglion. From there, it exits the skull through the foramen ovale and branches out to different regions of the face and jaw. The nerve is composed of both sensory and motor fibers, which allow for the transmission of signals and coordinated movement.
As the mandibular nerve travels through the foramen ovale, it gives rise to various branches that supply sensation to different areas of the face. These branches include the mental nerve, which provides sensation to the chin and lower lip, and the buccal nerve, which innervates the cheek region. The intricate network of branches highlights the extensive reach and importance of the mandibular nerve in facial sensation.
Functions of the Mandibular Nerve
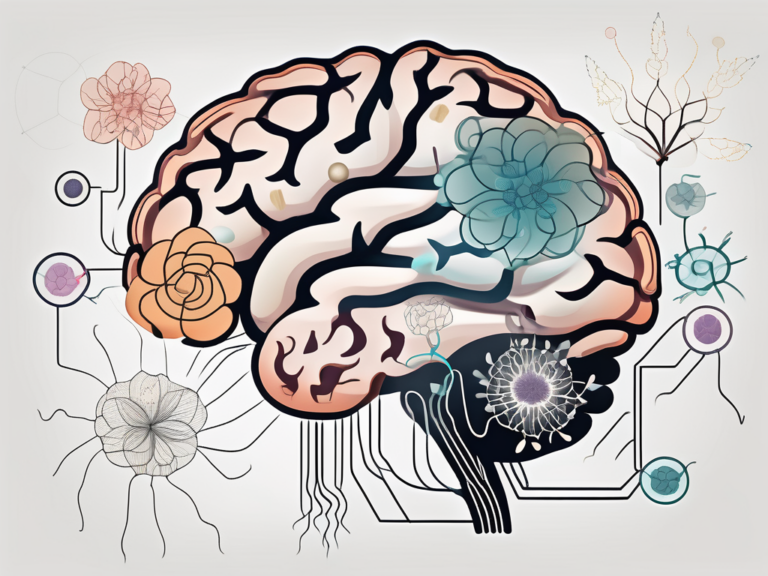
The primary function of the mandibular nerve is to transmit sensory information from the lower face and jaw to the brain. This includes sensations of touch, temperature, and pain. Additionally, the mandibular nerve innervates the muscles responsible for biting and chewing, ensuring proper functioning of the jaw.
Moreover, the mandibular nerve plays a crucial role in the reflex mechanisms involved in protecting the oral cavity. When stimulated, this nerve can initiate reflex actions that help prevent injury to the teeth and surrounding structures. This intricate system of sensory and motor functions showcases the mandibular nerve’s significance in maintaining oral health and facilitating essential daily activities.
The Mandibular Nerve and Oral Health
Several aspects of oral health are directly influenced by the mandibular nerve. Dental professionals rely on a thorough understanding of the nerve to perform procedures effectively, and any disruption to its functioning can have implications for speech and eating.
The mandibular nerve, also known as the inferior alveolar nerve, is a branch of the trigeminal nerve responsible for providing sensory innervation to the lower teeth, gums, and lip. It travels through the mandibular foramen and into the mandibular canal, where it branches out to supply sensation to the lower jaw. This intricate network of nerves is vital for maintaining oral health and function.
Role in Dental Procedures
During dental procedures, such as extractions or root canals, dentists must work with precision to avoid damaging the mandibular nerve. Accidental injury to the nerve can lead to temporary or even permanent loss of sensation in the lower face, impacting a patient’s quality of life. Therefore, dentists carefully consider the anatomical pathway of the nerve when planning and executing treatments.
Advanced imaging techniques, such as cone beam computed tomography (CBCT), are often used to visualize the exact location of the mandibular nerve before surgical interventions. This technology allows for precise treatment planning and reduces the risk of nerve injury during complex dental procedures.
Impact on Speech and Eating
The mandibular nerve plays a crucial role in proper speech and eating. Changes in nerve function or damage can result in difficulties in articulating certain sounds and swallowing food effectively. Individuals with mandibular nerve disorders may experience numbness, tingling, or even pain in the lower face, making it challenging to perform everyday activities such as eating and speaking with ease.
Speech therapists and oral health professionals often collaborate to help patients with mandibular nerve issues regain optimal function. Through targeted exercises and therapies, individuals can improve their speech articulation and swallowing abilities, enhancing their overall quality of life.
Disorders Related to the Mandibular Nerve
Various disorders can affect the normal functioning of the mandibular nerve. Recognizing the symptoms and seeking appropriate diagnosis and treatment are essential for managing these conditions.
The mandibular nerve, also known as the inferior alveolar nerve, is a branch of the trigeminal nerve responsible for providing sensory innervation to the lower teeth, gums, and lip. It plays a crucial role in the proper functioning of the jaw and facial muscles, making any disorders affecting it significant and potentially debilitating.
Symptoms of Mandibular Nerve Disorders
Mandibular nerve disorders may manifest as pain in the lower face, jaw joint disorders, sensitivity or numbness in the lower lip, or difficulty chewing and speaking. Additionally, patients may experience referred pain from the nerve, leading to headaches or neck pain. Recognizing these symptoms and seeking timely medical attention is crucial for effective management.
In some cases, mandibular nerve disorders can also result in a condition known as trigeminal neuralgia, characterized by sudden, severe facial pain resembling an electric shock. This excruciating pain can be triggered by simple activities such as talking, eating, or even a light touch to the face, significantly impacting the quality of life for those affected.
Diagnosis and Treatment Options
Diagnosing mandibular nerve disorders requires a thorough examination and medical history assessment. Dental professionals, neurologists, or oral and maxillofacial specialists may perform various tests, including imaging, electromyography, or nerve conduction studies. Treatment options can range from medications to relieve pain and nerve blocks to surgical interventions in severe cases. It is essential to consult with a healthcare professional to determine the most appropriate course of action.
Furthermore, in cases where conservative treatments do not provide adequate relief, advanced procedures such as radiofrequency ablation or microvascular decompression surgery may be considered to alleviate the debilitating symptoms and improve the patient’s quality of life. Each treatment approach is tailored to the individual’s specific condition and response to previous interventions, highlighting the importance of personalized care in managing mandibular nerve disorders.
The Mandibular Nerve and Pain Management
Pain management is a key aspect of dentistry and medicine in general. Understanding the role of the mandibular nerve in pain perception and implementing techniques to alleviate pain are of utmost importance to provide effective patient care.
The mandibular nerve, a branch of the trigeminal nerve, plays a crucial role in transmitting sensory information from the lower jaw, teeth, and gums to the brain. This nerve is responsible for providing sensation to the lower teeth and gums, as well as the lower lip and chin. Dysfunction of the mandibular nerve can result in various types of orofacial pain, including sharp shooting pain, tingling, or numbness in the lower face.
Understanding Trigeminal Neuralgia
One of the most well-known conditions associated with the mandibular nerve is trigeminal neuralgia. This chronic pain disorder is characterized by severe facial pain, often triggered by simple actions like eating or talking. By understanding the specific pathways of the mandibular nerve, healthcare professionals can develop targeted treatment plans to alleviate pain and improve the quality of life for individuals with this condition.
Trigeminal neuralgia can be debilitating, impacting a person’s ability to perform daily activities and significantly reducing their quality of life. It is essential for healthcare providers to conduct a thorough evaluation to determine the underlying cause of trigeminal neuralgia, as treatment approaches may vary depending on whether the pain is due to compression of the nerve by a blood vessel or other structural abnormalities.
Techniques for Alleviating Mandibular Nerve Pain
Various techniques can be employed to alleviate mandibular nerve pain. These may include medications, nerve blocks, physical therapy, or even surgical interventions in severe cases. It is crucial for healthcare professionals to consider a multidisciplinary approach, tailoring treatments to individual patients based on the underlying cause and severity of their symptoms.
In addition to traditional pain management techniques, complementary therapies such as acupuncture, chiropractic care, and biofeedback may also be beneficial in managing mandibular nerve pain. These alternative approaches focus on addressing the body’s natural healing mechanisms and promoting overall well-being, offering patients a holistic approach to pain relief.
Future Research on the Mandibular Nerve
The study of the mandibular nerve holds promise for future advancements in regenerative medicine and understanding the impact of aging on nerve function.
Potential for Regenerative Medicine
Regenerative medicine aims to restore or replace damaged tissues using various techniques, including stem cell therapy. Research into the regenerative potential of the mandibular nerve may pave the way for innovative treatment options, particularly for individuals with nerve injuries or degenerative diseases.
The Mandibular Nerve and Aging
Aging can affect the overall function of nerves, including the mandibular nerve. Research focused on understanding age-related changes in nerve function can contribute to the development of strategies to maintain oral health and manage associated disorders effectively.
Exploring the regenerative capabilities of the mandibular nerve involves investigating how different types of stem cells can be utilized to repair nerve damage. By understanding the specific mechanisms involved in nerve regeneration, researchers can tailor treatments to optimize outcomes and potentially reverse nerve dysfunction.
Moreover, the potential applications of regenerative medicine in mandibular nerve injuries extend beyond physical restoration. There is growing interest in exploring how regenerative techniques can also address sensory deficits and improve overall nerve function, offering a holistic approach to nerve injury management.